
Understanding Folliculitis: Causes, Symptoms, and Treatment Options
Folliculitis is a common skin condition that arises from the inflammation of hair follicles. It can occur anywhere on the body where hair grows, leading to red, inflamed bumps or pustules that are often itchy or painful. This blog aims to provide a comprehensive understanding of folliculitis, its causes, how it can be treated, and preventative measures one can take.
What is Folliculitis?
Folliculitis occurs when hair follicles become inflamed due to bacterial, fungal, or viral infections. It can also be caused by irritation from shaving, certain clothing, or other frictional forces. While usually not serious, folliculitis can be uncomfortable and lead to more severe infections or scarring if not appropriately managed.
Types of Folliculitis
Folliculitis can be classified mainly into two categories: superficial and deep. Both vary in terms of symptoms and severity.
- Superficial Folliculitis: Affects the upper part of the hair follicle. It appears as clusters of small red bumps or pus-filled blisters surrounding hair follicles. Common types include:
- Bacterial Folliculitis: Often caused by Staphylococcus aureus bacteria.
- Hot Tub Folliculitis: Caused by Pseudomonas bacteria, often from improperly chlorinated hot tubs or pools.
- Deep Folliculitis: Involves the entire hair follicle and is typically more severe. It can cause larger sores and may lead to scarring. Types include:
- Barber’s Itch (Pseudofolliculitis barbae): Common in people who shave, especially in the beard area.
- Sycosis Barbae: A chronic form that affects the entire hair-growing area.
Symptoms and Recognition
Symptoms of folliculitis can vary depending on the severity and type, but often include:
- Clusters of small red or pus-filled bumps.
- Itchy or burning skin.
- Presence of pimples around hair follicles.
- Tender skin with possible swelling.
- In severe cases, large swollen bumps and crusty sores.
Causes and Risk Factors
The exact cause of folliculitis often dictates the appropriate treatment approach.
- Infections: Staphylococcus aureus is a common bacterial cause, while fungi such as Candida can also lead to infection.
- Friction and Irritation: Tight clothing, frequent shaving, or improperly used hot tubs.
- Obstructed Follicles: Caused by oil, dead skin cells, and sweat.
- Weakened Immune System: Conditions like diabetes or HIV can increase susceptibility.
Risk factors include poor shaving techniques, wearing tight clothing, exposure to dirty water or spa facilities, excessive sweating, and having certain skin conditions.
How Contagious is Folliculitis?
Folliculitis caused by infectious agents can be contagious and spread through skin-to-skin contact or sharing of personal items such as razors, towels, or clothing.
Diagnosis and Tests
A healthcare provider typically diagnoses folliculitis through a physical examination and reviewing the symptoms. In cases where common treatments fail, a culture or skin biopsy may be taken to identify the specific cause of infection.
Management and Treatment
Treatment usually depends on the type and severity of folliculitis. Most cases resolve with basic self-care and preventive measures:
Home Remedies
- Warm Compresses: Applying warm, moist compresses can provide relief from itching and draw out pus.
- Proper Hygiene: Regularly washing the affected area with anti-bacterial soap.
Over-the-Counter Treatments
- Topical Antibiotic Ointments such as Neosporin®.
- Antifungal Creams for Candida-related folliculitis.
Prescription Medications
If severe or recurrent, physicians may prescribe:
- Oral Antibiotics: For bacterial infections. Learn more
- Antiviral Drugs: If herpes simplex virus is involved.
- Antifungal Medications: For chronic yeast folliculitis.
Procedures
- Laser Hair Removal: Can prevent future folliculitis related to shaving.
- Minor Surgery: Draining large boils caused by deep folliculitis.
Prevention of Folliculitis
Preventive practices can minimize the risk or severity:
- Good Personal Hygiene: Daily cleansing and avoiding the sharing of personal care items.
- Proper Shaving Techniques: Use of sharp blades and shaving in the direction of hair growth.
- Clothing Choices: Avoiding tight and non-breathable fabrics.
- Hot Tubs and Pools: Ensure proper sanitation or shower immediately after use.
When to See a Doctor
Though self-care and OTC treatments often work, seeing a healthcare provider is essential if the condition does not improve, worsens, or symptoms such as fever or spreading lesions develop.
Frequently Asked Questions
Is Folliculitis Contagious?
Yes, especially if caused by bacterial or viral infections. Avoid sharing towels and personal items until the infection is under control.
Can Folliculitis Lead to Other Complications?
Chronic folliculitis can lead to scarring and skin discoloration. Severe infections might result in boils or abscesses.
Should People With Folliculitis Avoid Shaving?
It's advisable to stop shaving if you have active folliculitis until the infection clears to avoid further irritation.
Additional Resources
For more detailed information about folliculitis, its causes, and treatments, consider these resources:
Understanding folliculitis is crucial for effective management and prevention. Following the guidelines and treatments prescribed by healthcare professionals can lead to better skin health and avoid complications.
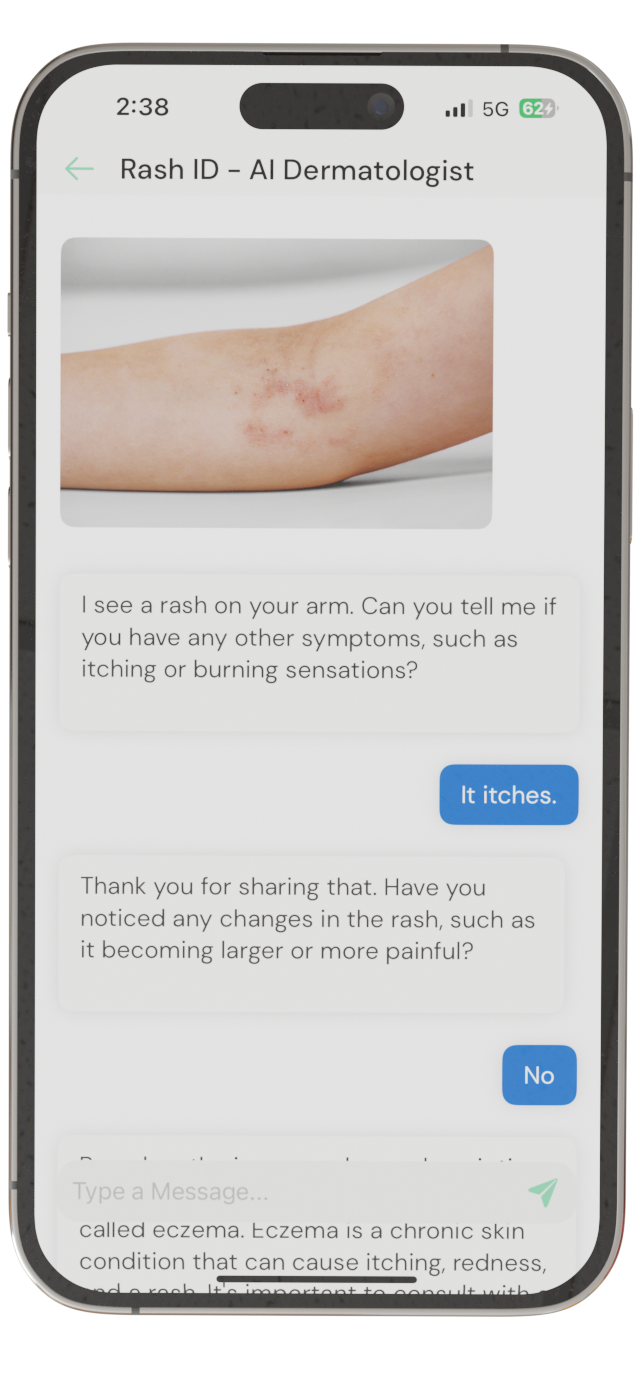
Identify Skin Conditions Instantly
Try Rash ID for Free