
Understanding Hives: Causes, Symptoms, and Treatment
Hives, also known as urticaria, are itchy, raised welts on the skin that can be uncomfortable and distressing. They are a common allergic reaction, whose triggers can vary widely. It's essential to understand hives comprehensively, especially if you or someone you know frequently experiences them.
What are Hives?
Hives are a kind of skin rash notable for pale red, raised, and itchy bumps. They result from the body's reaction to certain allergens, which cause the skin to react. Hives can be acute or chronic, lasting from a few hours to several months. Unlike other skin rashes, hives are characterized by their transient nature, meaning they appear and fade repeatedly as the reaction progresses.
Types of Hives
- Acute Urticaria: These hives last less than six weeks and are typically brought on by pressure from tight clothing, sun exposure, exercise, infections, or allergic reactions to food or medicine.
- Chronic Urticaria: These hives last over six weeks and can persist for months or years. They are less often linked to allergens and are instead thought to involve an autoimmune component.
- Physical Urticaria: Triggered by physical stimuli such as temperature changes, sun exposure, water, pressure, vibration, or exercise.
Recognizing Hives: Symptoms and Visual Clues
Recognizing hives is the first step in managing them effectively. Here are some common features:
- Raised Welts: Hives appear as raised, red or skin-colored welts that can happen anywhere on the body.
- Itching: The rash associated with hives is often very itchy, leading people to search for descriptions like "itchy skin rash" or "itchy red welts."
- Variable Size: They can vary in size from small dots to larger patches, even joining together to form plaques.
- Changing Shape and Location: Hives can change size and shape and may move around, disappearing from one spot and reappearing elsewhere.
Who Gets Hives?
Hives can affect anyone; however, they are more common in people with sensitivities to certain triggers:
- Allergies to foods, insects, or environmental factors.
- Sensitivity to temperature changes or physical stimuli.
- Underlying autoimmune conditions.
Symptoms and Causes
What are the Signs of Hives?
- Swollen, itchy welts with well-defined edges.
- Welts that change shape, size, and location.
- Flares that worsen with stress, heat, and certain foods or medications.
What Causes Hives?
Hives can have various triggers, such as:
- Allergens: Foods like nuts, shellfish, eggs, and dairy can cause hives.
- Medications: Antibiotics, painkillers, and aspirin are known culprits.
- Infections: Certain viral infections can lead to hives.
- Environmental Factors: Sun, cold, pressure, and stress can all trigger outbreaks.
How Contagious are Hives?
Hives are not contagious. You cannot transmit them to another person through contact. However, the underlying allergic or irritant conditions might have implications for different individuals.
Diagnosis and Tests
How are Hives Diagnosed?
Diagnosis usually involves a physical examination and medical history review by a healthcare provider. In some cases, allergy testing can help identify specific triggers.
Management and Treatment
How are Hives Treated?
The goal of treating hives is to relieve symptoms while addressing the underlying cause, if known.
Antihistamines
Antihistamines are the most common treatment to relieve itching and reduce the rash. Over-the-counter options include:
- Loratadine (Claritin®),
- Cetirizine (Zyrtec®),
- Fexofenadine (Allegra®), and
- Diphenhydramine (Benadryl®).
Corticosteroids
In severe cases, oral corticosteroids like Prednisone may be prescribed for short-term relief. However, these should be used cautiously due to potential side effects.
Immunomodulators
For chronic hives, medications like Omalizumab (Xolair®) may be used to modulate the immune system.
Home Care and Lifestyle Adjustments
- Avoid known triggers by identifying and steering clear of foods or activities that aggravate your condition.
- Use soothing lotions or cool compresses to calm the skin.
- Wear loose, lightweight clothing to reduce irritation.
- Manage stress through mindfulness, relaxation techniques, or yoga.
Prevention
How can I Prevent Hives?
While preventing hives entirely can be challenging, the following strategies may help reduce their frequency:
- Keep a record of when you get hives to identify patterns or triggers.
- Avoid known allergens, and consider an elimination diet if food allergies are suspected.
- Protect your skin from extreme temperatures, including sun exposure and cold weather.
Outlook / Prognosis
Can Hives Come Back?
Yes, hives can recur, especially if their underlying cause isn't properly managed. Chronic hives may last a year or longer but often resolve on their own eventually.
What are the Complications of Hives?
In rare situations, severe allergic reactions known as anaphylaxis must be treated as a medical emergency, requiring an immediate injection of epinephrine.
Living With Hives
When should I call the doctor?
Contact a healthcare provider if hives:
- Are accompanied by breathing difficulties or swelling of the throat (these are signs of anaphylaxis).
- Persist beyond a few weeks.
- Occur frequently without a known cause.
What questions should I ask my doctor?
- What do you suspect is triggering my hives?
- Are there specific tests that can be performed to identify the cause of my hives?
- Should I make any lifestyle changes to prevent future episodes?
- Are there alternative or additional treatments you would recommend?
- How should I handle hives if they appear unexpectedly?
Additional Common Questions
How are hives different from eczema?
Although both can cause itchy skin, hives are raised welts that move around, whereas eczema is more persistent and leads to scaly, red patches.
Can you develop immunity to hives or outgrow them?
While some children may outgrow hives associated with allergies, others may continue to experience them into adulthood due to different triggers.
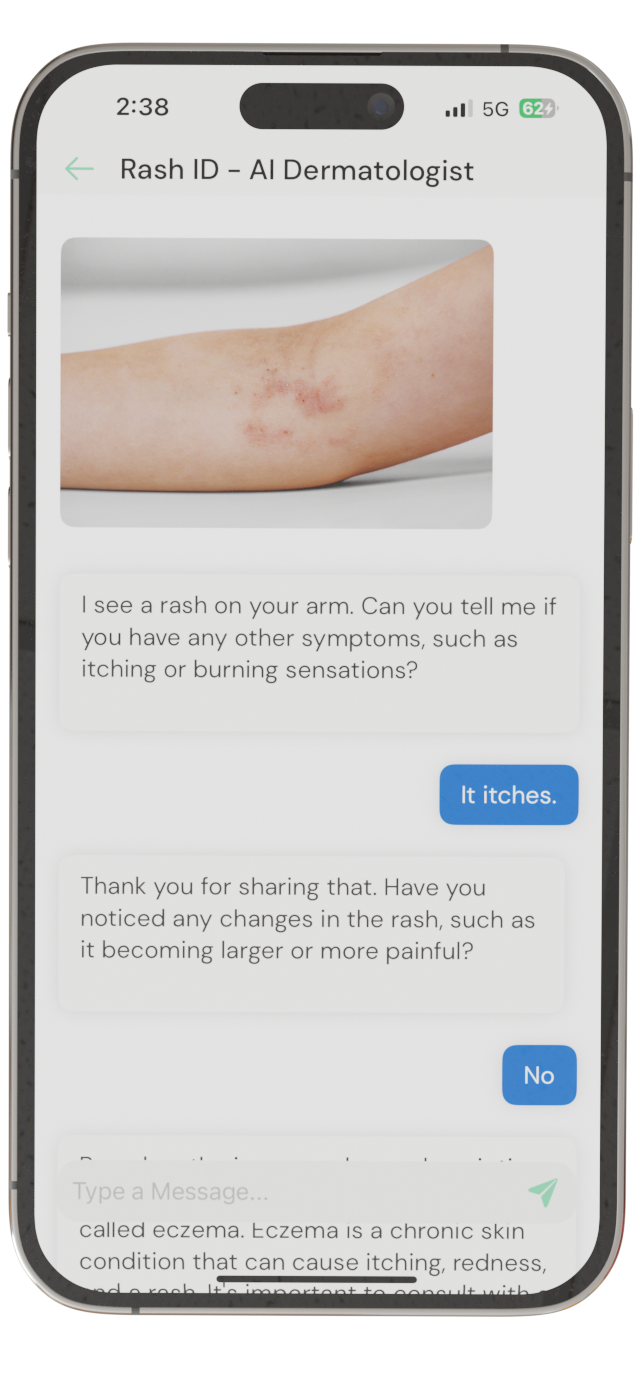
Identify Skin Conditions Instantly
Try Rash ID for Free