
Understanding Impetigo: Diagnosis, Symptoms, and Treatments
Impetigo is a common and highly contagious bacterial skin infection that primarily affects infants and young children, although it can occur in individuals of any age. The condition is characterized by red sores on the face, especially around a child’s nose and mouth, and on hands and feet. These sores burst and develop honey-colored crusts.
What is Impetigo?
Impetigo is primarily caused by two types of bacteria: Staphylococcus aureus and Streptococcus pyogenes (group A Streptococcus). It mostly occurs during the warmer months when conditions are more conducive to bacterial growth. The infection can spread rapidly through close contact or shared items like towels, clothes, and toys.
Types of Impetigo
- Non-bullous Impetigo: This is the most common type and begins as small red spots that quickly develop into blisters. These blisters rupture and leave behind honey-colored crusts.
- Bullous Impetigo: This type results in larger blisters that can appear on various parts of the body, including the trunk and diaper area in infants. The blisters are filled with a clear fluid and tend to remain unbroken longer.
- Ecthyma: A severe form of impetigo, ecthyma penetrates deeper into the skin than other forms and results in painful ulcers.
How to Recognize Impetigo: Symptoms and Visual Clues
Being familiar with the symptoms of impetigo is crucial for early detection and treatment:
- Red Sores: Small red spots or bumps that may itch and are usually found on the face.
- Blisters: Clusters of tiny fluid-filled vesicles that eventually burst and form a crust.
- Honey-colored Crusts: These crusts appear after the blisters break, are highly characteristic of impetigo, and often lead individuals to seek treatment.
- Itching and Soreness: The affected skin is frequently itchy and may be tender to the touch.
- Swollen Lymph Nodes: In some cases, nearby lymph nodes may swell as a response to the infection.
Who Gets Impetigo?
Impetigo affects people across all age groups but is more common in:
- Children: Especially those aged 2 to 5 years, due to their frequent close contact in settings such as schools and daycare centers.
- Athletes: Participants in sports that involve skin-to-skin contact, like wrestling.
- People with Skin Injuries: Those with cuts, insect bites, or other injuries are more susceptible as bacteria easily penetrate through breaks in the skin.
- Individuals with Eczema or Dermatitis: Those with pre-existing skin conditions that impair the skin barrier.
How Common is Impetigo?
Impetigo is one of the most common skin infections in children globally. It accounts for about 10% of all pediatric skin issues and affects millions of children each year.
Symptoms and Causes
Signs of Impetigo
Signs typically appear one to three days after infection. Common indicators include:
- Red, itchy sores around the nose and mouth.
- Blisters that pop and crust over.
- Occasionally, systemic symptoms like fever for severe cases.
Causes of Impetigo
The main contributing factors are the infection with Staphylococcus aureus or Streptococcus pyogenes bacteria that enter the skin through minor cuts, insect bites, or other abrasions.
Diagnosis and Tests
A healthcare provider can often diagnose impetigo based on its distinctive appearance. In some cases, they might take a swab of the blisters or crust to identify the exact type of bacteria causing the infection and determine the most effective antibiotic.
Management and Treatment
How is Impetigo Treated?
Impetigo can typically be treated effectively with antibiotics. The treatment will depend on the severity and extent of the infection.
Topical Antibiotics
Mild cases can often be treated with prescription topical antibiotics. These may include:
- Mupirocin (Bactroban®): A common cream used for treating impetigo.
- Retapamulin (Altabax®): Used for small areas of affected skin.
Oral Antibiotics
Severe or more widespread impetigo may require oral antibiotics like:
- Cephalexin (Keflex®)
- Dicloxacillin
For penicillin-allergic individuals or cases caused by methicillin-resistant Staphylococcus aureus (MRSA), alternative antibiotics like Clindamycin or Trimethoprim-sulfamethoxazole (Bactrim®) might be utilized.
Home Care Methods
Proper skin hygiene plays a crucial role in managing impetigo. Care steps include:
- Gently washing the infected area with soap and water.
- Keeping nails short to prevent scratching and spreading the infection.
- Using separate towels and washcloths for affected individuals.
Prevention
The following strategies can help prevent the spread of impetigo, especially in households or schools:
- Hand Hygiene: Regular and thorough washing of hands with soap and water.
- Avoiding Close Contact: Keeping those infected away from school or daycare until 24 hours after starting antibiotics.
- Not Sharing Personal Items: Avoid sharing towels, clothing, or any personal items with others.
Outlook / Prognosis
With treatment, impetigo typically resolves completely without scarring. In rare cases, complications such as post-streptococcal glomerulonephritis can occur, which affects the kidneys.
Living With
When to Call the Doctor
Contact your healthcare provider if:
- The sores do not improve after 3 days of prescribed antibiotic treatment.
- Signs of infection such as fever or increased redness and swelling occur.
- Impetigo spreads to other body parts or other household members become infected.
Additional Common Questions
Is impetigo contagious?
Yes, impetigo is highly contagious and can be easily transmitted between individuals through direct contact with sores or contact with items used by someone infected.
How long does impetigo last?
With proper treatment, impetigo generally clears up in about 7 to 10 days. Without treatment, it can persist for weeks and may lead to more severe conditions.
For further information, you can visit CDC’s impetigo page or Mayo Clinic’s overview on impetigo.
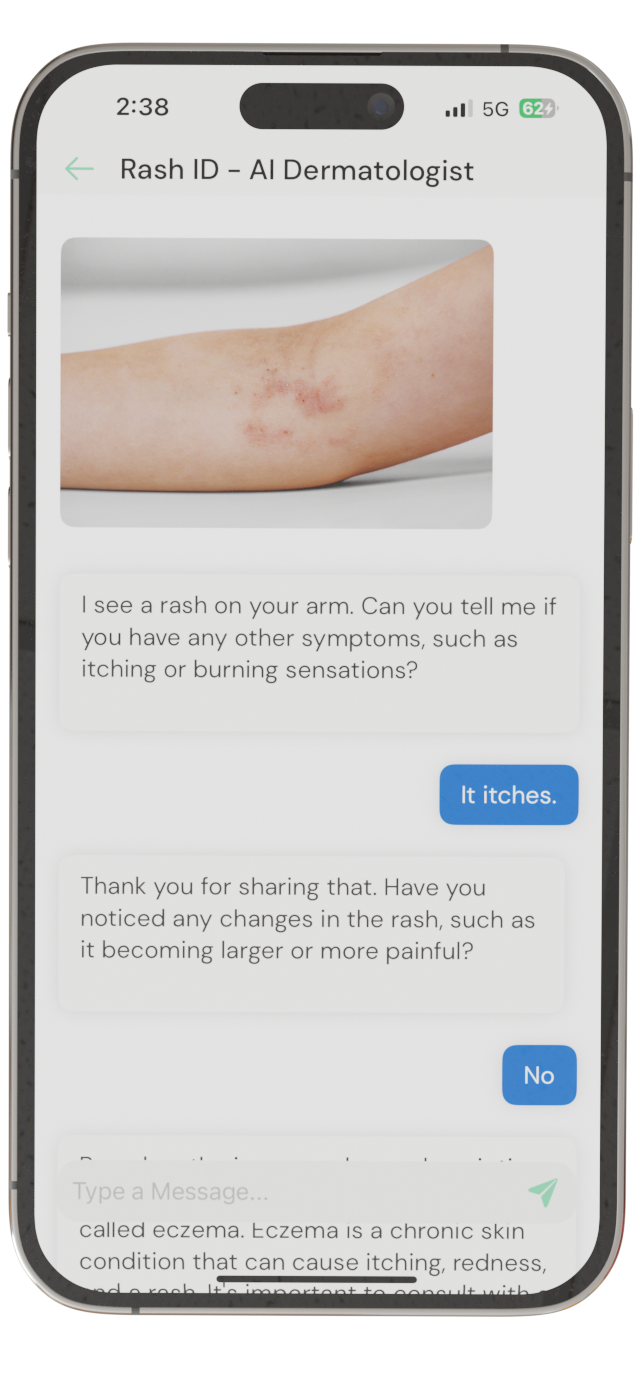
Identify Skin Conditions Instantly
Try Rash ID for Free