
Understanding Psoriasis: Causes, Symptoms, and Treatments
What is Psoriasis?
Psoriasis is a chronic autoimmune condition that causes the rapid buildup of skin cells, leading to scaling on the skin’s surface. The formation of scales and red patches is common, and they often produce itching and sometimes pain. This condition, which can fluctuate between periods of remission and flare-ups, affects roughly 2-3% of the global population.
Psoriasis is not contagious, and its exact cause is multifactorial, including genetics and environmental factors. It is often associated with other health conditions such as psoriatic arthritis, cardiovascular disease, and anxiety or depression.
For a detailed overview of psoriasis, visit the National Psoriasis Foundation.
Types of Psoriasis
There are several types of psoriasis, each characterized by different symptoms and requiring unique approaches to treatment.
- Plaque Psoriasis (Psoriasis Vulgaris): The most common form, accounting for about 80-90% of cases. It leads to dry, raised, red skin lesions (plaques) covered with silvery scales. You'll often find these on the elbows, knees, scalp, and lower back.
- Guttate Psoriasis: Often starts in childhood or young adulthood, characterized by small, water-drop-shaped, scaling lesions on the trunk, limbs, and scalp.
- Inverse Psoriasis: Causes bright red, shiny lesions that appear in skin folds, such as under the breasts, in the groin, or around the genitals and buttocks.
- Pustular Psoriasis: A rarer form characterized by white pustules (blisters of non-infectious pus) surrounded by red skin. It can be localized to certain areas or widespread.
- Erythrodermic Psoriasis: The least common but most severe form that can cover a large area of the body with a red, peeling rash that can itch or burn intensely.
Symptoms and Recognition
Psoriasis symptoms vary by type but typically include:
- Red patches of skin covered in thick silver scales: Common in plaque psoriasis.
- Dry, cracked skin that may bleed: The build-up of skin cells forms white-silver scales and red patches, which can become cracked and bleed.
- Itching, burning, or soreness: Frequent around the affected areas.
- Nail problems: Psoriatic nail dystrophy can affect both fingernails and toenails, leading to pitting, abnormal nail growth, and discoloration.
- Swollen and stiff joints: Sometimes indicative of psoriatic arthritis.
Who Gets Psoriasis?
Psoriasis can affect anyone, but several risk factors might increase the likelihood of developing the disease:
- Genetics: Family history plays a crucial role. If one or both parents have psoriasis, the risk is higher.
- Infections and Skin Injuries: Throat infections, such as strep throat, can trigger guttate psoriasis. Cuts, bug bites, severe sunburn, or a vaccination could start an outbreak.
- Lifestyle Factors: Stress, smoking, and heavy alcohol consumption might worsen symptoms.
- Medications: Some drugs, including lithium, antimalarial drugs, or certain high blood pressure medications, may trigger psoriasis.
Diagnosis and Tests
Diagnosing psoriasis typically involves a physical examination of the skin, scalp, and nails. In uncertain cases, your healthcare provider might perform a biopsy where a small sample of skin is examined under a microscope.
For further guidance, visit the American Academy of Dermatology’s page on psoriasis diagnosis.
Management and Treatment
The treatment plan is personalized and depends on the severity and type of psoriasis, including:
- Topical treatments: These are the first line of treatment for mild to moderate psoriasis. They include corticosteroids, vitamin D analogues, anthralin, and topical retinoids.
- Phototherapy: Also known as light therapy, this treatment involves exposing the skin to ultraviolet light on a regular schedule and under medical supervision.
- Systemic medications: Taken orally or by injection, these are usually reserved for severe psoriasis due to their potential side effects.
- Methotrexate, Cyclosporine, Biologics: These medications can suppress the immune system and control inflammation.
- Biological treatments can be particularly effective in managing psoriasis and psoriatic arthritis.
- Natural remedies and lifestyle changes: Moisturizing, using aloe vera, reducing stress, and maintaining a healthy diet can ease symptoms. Fish oil supplements and vitamin D are often recommended, but always discuss with your healthcare provider first.
For a more comprehensive list of treatments, the Mayo Clinic provides detailed explanations and options.
Prevention and Management
While psoriasis cannot be cured, its symptoms can be managed through:
- Maintaining a healthy lifestyle: This includes eating a balanced diet, quitting smoking, reducing alcohol intake, and exercising regularly.
- Skin Care: Moisturizing regularly, avoiding harsh soaps, and taking care of your skin and scalp can help reduce outbreaks.
- Reducing Stress: Stress management techniques, such as yoga, meditation, or therapy, can help minimize flare-ups.
Living With Psoriasis
The chronic nature of psoriasis means that managing and living with this condition necessitates long-term care and attention. Regular consultations with a dermatologist or healthcare provider are crucial. Open communication can lead to a more effective treatment plan tailored to your needs.
Additional Common Questions
Is Psoriasis Associated with Arthritis?
Yes, approximately 30% of people with psoriasis may also develop psoriatic arthritis, an inflammatory condition that affects the joints. Click here for more information.
Can Diet Affect Psoriasis?
While no specific diet can cure psoriasis, some dietary changes (like reducing sugar and managing weight) may improve symptoms. Further evidence is detailed by the National Psoriasis Foundation’s guidelines on diet.
Are There Triggers for Psoriasis Flare-ups?
Common triggers include stress, injury to the skin, certain medications, and infections like strep throat. Identifying and managing these triggers can help control flare-ups. For more, visit the American Academy of Dermatology on psoriasis triggers.
Embracing education and understanding about psoriasis can greatly improve one's quality of life and help manage this long-term condition effectively. Consult healthcare professionals for the most personalized and effective treatment strategies.
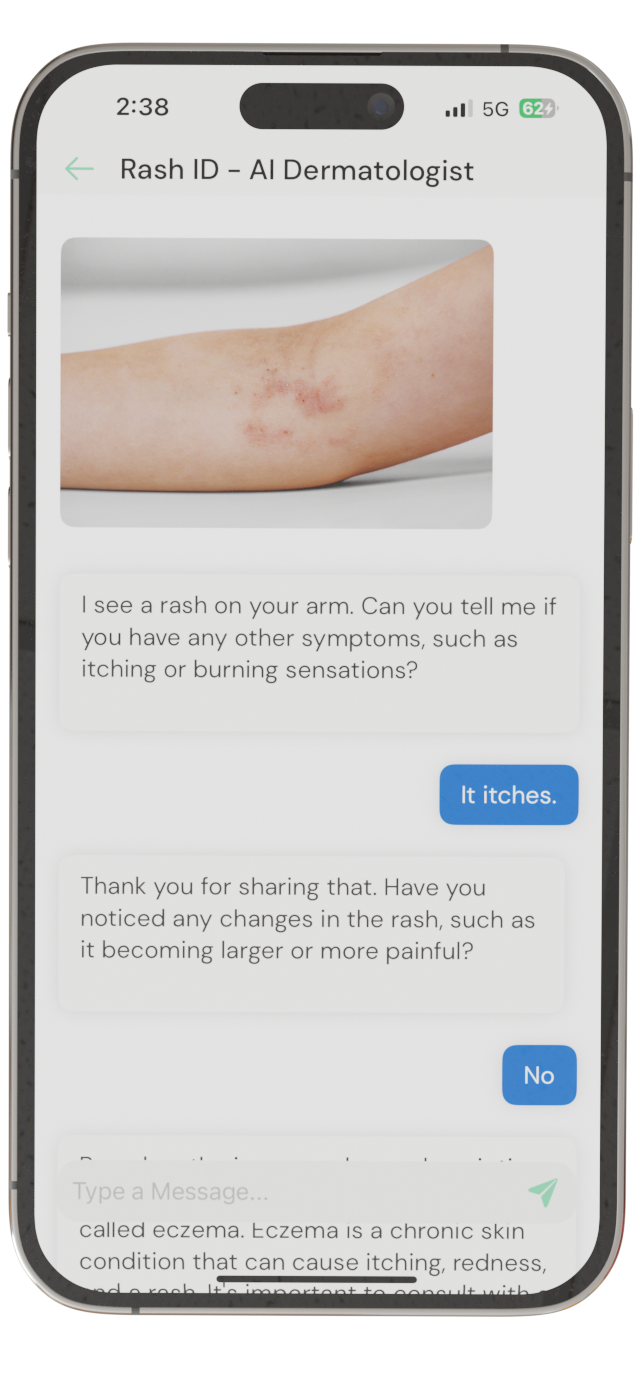
Identify Skin Conditions Instantly
Try Rash ID for Free