Overview
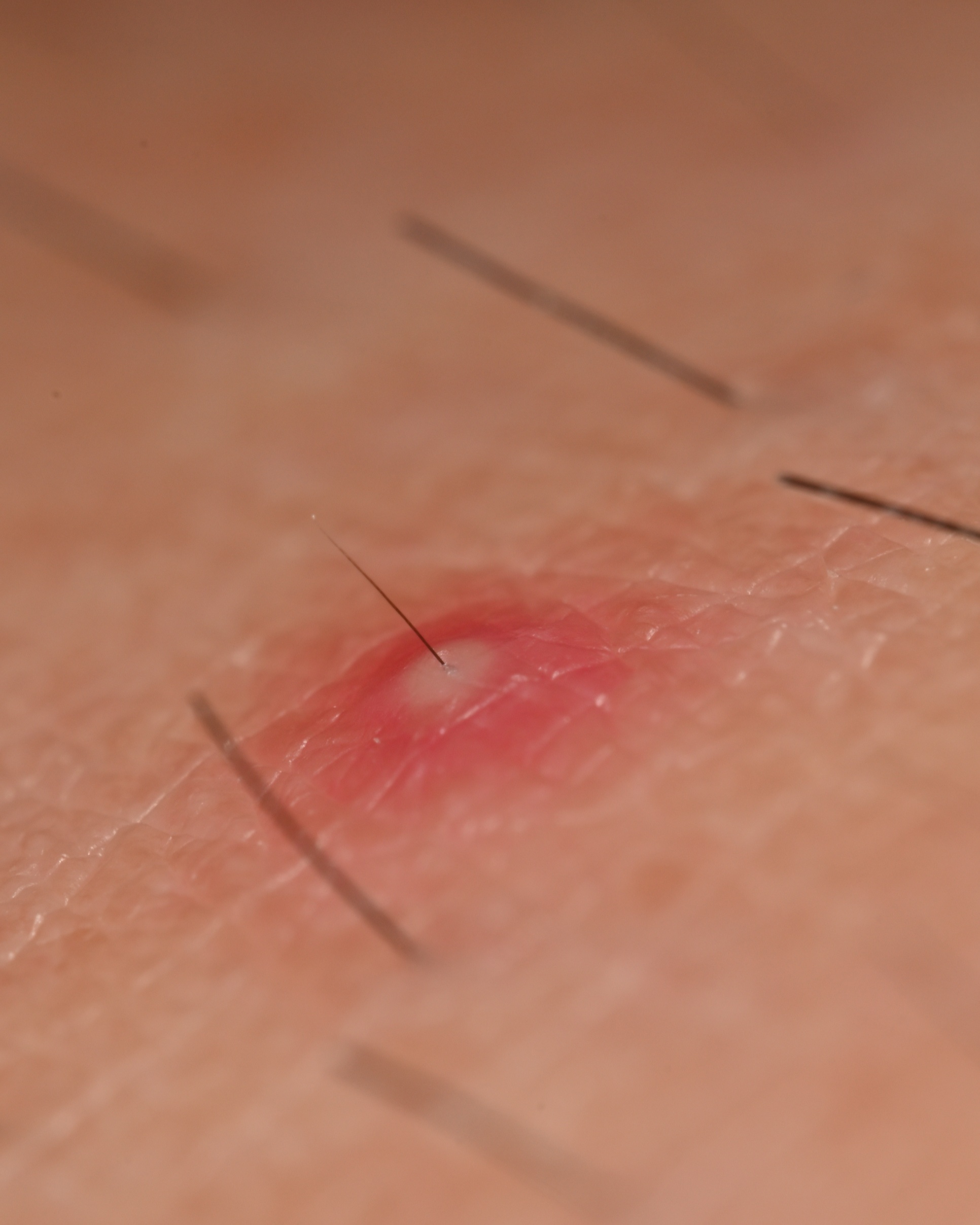
Folliculitis is a common skin condition where hair follicles, the tiny pockets in your skin where hair grows from, become inflamed. It often looks like small, red, tender bumps or white-headed pimples around these follicles, and sometimes a hair can be seen in the middle of a bump.
It's most often caused by a bacterial infection (like Staphylococcus aureus, or "staph"), but fungi, viruses, irritation from shaving, friction from tight clothing, or even ingrown hairs can also be the culprit. Anyone can get folliculitis, from children to adults, and it's particularly common in people who shave, wax, wear tight clothing that rubs the skin, or use hot tubs.
A common question we hear, especially from parents, is: Is it contagious? Some types of folliculitis, particularly those caused by bacteria or fungi, can be spread through close skin contact, sharing personal items like razors or towels, or through contaminated water in hot tubs or pools. While often just a nuisance, folliculitis can be itchy, sore, and sometimes make you feel self-conscious. We understand that dealing with any skin issue can be frustrating.
Symptoms
You might be experiencing folliculitis if you notice:
- Clusters of small red bumps or little white-headed pimples - that form around hair follicles.
- Each pimple - might have a hair shaft visible in its center.
- Pus-filled blisters - that can break open and then form a crust.
- Itching, burning, or a stinging sensation - in the affected skin area.
- Tenderness or pain - around the bumps.
- In some cases, especially with deeper folliculitis, larger swollen bumps or even boils (furuncles) - can form.
- These symptoms - can appear anywhere on your body where hair grows, including your scalp, face (especially the beard area), neck, armpits, chest, back, buttocks, arms, and legs.
- Symptoms - might seem to flare up or get worse after shaving, wearing tight clothes, or sweating a lot.
Diagnosis
Figuring out if you have folliculitis usually starts with a close look at your skin. A healthcare professional can often diagnose it simply by examining the affected areas and talking with you about your symptoms, your daily habits (like shaving or hot tub use), and your medical history.
Sometimes, to pinpoint the exact cause, especially if it's a persistent or severe case, your doctor might gently take a swab from one of the pustules. This sample is then sent to a lab to check for bacteria or fungi. In rarer situations, if the diagnosis isn't clear or the condition isn't improving, a small skin sample (a biopsy) might be taken for a closer look under a microscope.
Treatment
Finding the right treatment for folliculitis depends on the cause and severity of your condition. The good news is that many mild cases can be managed at home, while more persistent cases often respond well to medical treatment.
Over-the-Counter (OTC) Options:
For mild folliculitis, you can start with some simple at-home care. Look for products with these ingredients:
- Benzoyl peroxide: This is a great ingredient to fight bacteria. You can find it in washes, foams, and gels.
- Salicylic acid: This helps to exfoliate the skin and unclog pores.
- Hydrocortisone cream: If your skin is itchy, a non-prescription hydrocortisone cream can provide some relief.
Home Care and Self-Management:
A little extra care at home can go a long way in helping your skin heal and preventing future flare-ups:
- Warm Compresses: Applying a warm, moist washcloth to the affected area for 15-20 minutes a few times a day can help soothe the skin and encourage drainage of any pus-filled bumps.
- Gentle Cleansing: Wash the affected skin twice a day with an antibacterial soap or cleanser. Be gentle and avoid scrubbing, which can irritate your skin more.
- Avoid Irritation: Try to avoid shaving, waxing, or wearing tight clothing that rubs against the affected area until the folliculitis clears up.
- Keep it Clean: Use a clean towel and washcloth every time you wash. Wash towels, washcloths, and any clothing that comes into contact with the affected skin in hot, soapy water.
When Prescription Treatments May Be Needed:
If your folliculitis doesn't improve with at-home care, or if it's more severe, it's time to see a doctor. They may prescribe:
- Topical Antibiotics: These are creams, lotions, or gels that you apply directly to your skin to kill bacteria.
- Oral Antibiotics: For more widespread or deeper infections, you may need to take antibiotic pills.
- Antifungal Medications: If your folliculitis is caused by a fungus (like yeast), your doctor will prescribe antifungal creams, shampoos, or pills.
- Steroid Creams: For some types of folliculitis, a prescription-strength steroid cream can help reduce inflammation and itching.
Expected Timeline for Improvement:
With the right treatment, you should start to see improvement within a few days to a week. It's important to complete the full course of any prescribed medication, even if your skin starts to look better, to make sure the infection is completely gone.
Tips for Choosing the Right Treatment Approach:
- Start simple: For a few small bumps, try home care first.
- Pay attention to the cause: If you notice folliculitis after being in a hot tub, for example, it's likely caused by a specific type of bacteria and may clear up on its own.
- Don't hesitate to get help: If you're not sure what's causing your folliculitis or if it's getting worse, seeing a doctor is the best way to get an accurate diagnosis and the right treatment.
Important Safety Considerations and Warnings:
- Never pick or squeeze the bumps: This can make the infection worse, lead to scarring, and spread the bacteria to other parts of your body.
- Be careful with shaving: If you must shave, use a clean, sharp blade each time, shave in the direction of hair growth, and use a moisturizing shaving cream or gel.
- Always follow your doctor's instructions: Use medications as prescribed and for the full duration of treatment.
What to do if treatments aren't working:
If you've been treating your folliculitis for a couple of weeks and it's not getting better, or if it's getting worse, it's important to go back to your doctor. You may need a different medication or further testing to figure out what's going on. Living with any skin condition can be frustrating, but please know that with the right care, you can get it under control.
Duration & Outlook
Many mild cases of folliculitis can clear up on their own within a week or two, especially with good hygiene and by avoiding whatever might be irritating the skin. It can be an acute issue, meaning it's short-term, but for some individuals, it can become chronic (long-lasting) or keep coming back, particularly if the underlying triggers aren't managed.
The good news is that most of the time, folliculitis resolves without any lasting problems. However, more severe or deeper infections can sometimes lead to complications like scarring, permanent hair loss in the affected spots, or the infection spreading to nearby skin (cellulitis).
Warning signs for complications
that mean you should seek medical attention include the redness spreading quickly, the area becoming much more painful or swollen, developing a fever, or if the bumps turn into large, very painful boils (furuncles or carbuncles).
Prevention
Taking a few careful steps can often help prevent folliculitis from starting or coming back. We know it's not always easy, but these tips can make a difference:
- Try to wear loose-fitting clothing - especially when it's warm or when you're exercising, to reduce friction and allow your skin to breathe.
- If you shave, do so with care. - Use a clean, sharp razor blade each time (or consider disposable razors). Shave in the direction your hair grows, not against it, and use a moisturizing shaving cream, gel, or soap. Rinse with cool water and apply a soothing aftershave.
- Be cautious with hot tubs and heated swimming pools. - Only use ones that you know are well-maintained and properly chlorinated. It's a good idea to shower with soap and water as soon as you get out.
- Avoid sharing personal items - like towels, razors, and washcloths, as this can sometimes spread infections.
- Keep your skin clean - by washing regularly with a mild soap, especially after sweating.
Causes & Triggers
Understanding what might be causing or triggering your folliculitis is key. The most frequent cause is an infection by bacteria, particularly Staphylococcus aureus (staph bacteria), which normally live on the skin but can cause problems if they get into a damaged hair follicle. Other causes include:
- Fungal infections - (like those caused by yeast, sometimes called "Pityrosporum folliculitis" or "Malassezia folliculitis," often seen on the chest and back).
- Viruses - (though less common).
- Inflammation - from ingrown hairs, especially in areas that are shaved or waxed.
- Irritation - from substances like oils, tars, or certain topical medications.
Common triggers
that can damage follicles or introduce germs include:
- Shaving, waxing, or plucking hairs - These can damage the follicle opening.
- Friction - Tight clothing, backpack straps, or athletic gear rubbing against the skin.
- Excessive sweating - Sweat can irritate follicles, especially if trapped by clothing.
- Occlusive products - Heavy oils, thick moisturizers, or greasy ointments can block follicles.
- Hot tubs or whirlpools - "Hot tub folliculitis" is caused by Pseudomonas aeruginosa bacteria that thrive in warm, wet environments if chlorine levels aren't right.
- Certain skin conditions - Having dermatitis (eczema) or acne can sometimes increase your risk.
- Weakened immune system - Conditions like diabetes or HIV, or taking certain medications, can make you more prone to infections.
Anyone can develop folliculitis, but it's more common in people who shave frequently, athletes, those who wear tight clothing, individuals with oily skin or acne, or those with compromised immune systems.
When to see a doctor
While mild folliculitis might clear up with careful home care, it's important to know when to reach out to a healthcare professional. Please consider making an appointment if:
- The condition - is widespread over your body.
- It - doesn't start to improve after about a week or two of self-care measures.
- The bumps - are becoming increasingly painful, very itchy, or seem to be getting larger or deeper.
- You develop a fever - or start to feel generally unwell along with the skin symptoms.
- The folliculitis - keeps coming back frequently, despite your best efforts to prevent it.
- You notice signs - that the infection might be spreading, such as rapidly increasing redness, warmth, swelling, or streaks leading away from the affected area.
- You suspect - you have "hot tub folliculitis," as this often needs specific attention.
A doctor, and particularly a dermatologist, can accurately diagnose the cause of your folliculitis and discuss the best way forward if self-care isn't enough. It's always better to get things checked out if you're worried.
Frequently Asked Questions (FAQs):
- Q: Is folliculitis the same thing as acne? A: They can look similar, but they're different. Acne typically involves clogged pores (a mix of oil and dead skin cells leading to blackheads, whiteheads, and pimples), while folliculitis is specifically an inflammation or infection centered on the hair follicle itself. It's possible to have both.
- Q: Should I try to pop the bumps if I have folliculitis? A: It's really best to avoid squeezing, picking, or trying to pop the bumps. Doing so can actually make the inflammation worse, potentially spread bacteria deeper into the skin or to other follicles, and increase the risk of scarring or a more serious infection.
- Q: Can folliculitis leave scars on my skin? A: Mild folliculitis usually heals without leaving any scars. However, if the folliculitis is deeper, like with boils (furuncles), or if the bumps are repeatedly picked at or become severely infected, there is a chance of scarring or changes in skin color (darker or lighter patches) in that area.
- Q: If shaving seems to cause my folliculitis, do I have to stop shaving completely? A: Shaving is a very common trigger. If you notice a link, it might be helpful to stop shaving the affected area for a few weeks to allow the skin to heal and see if it improves. If you need to shave, make sure to follow all the preventive tips carefully, like using a clean, sharp blade, shaving with the grain of hair growth, and using a good shaving lubricant. Sometimes, exploring other hair removal methods might be an option.
- Q: What is "barber's itch"? Is that a type of folliculitis? A: Yes, "barber's itch" is a term often used to describe folliculitis that occurs in the beard area of the face and neck. It can be caused by ingrown hairs (pseudofolliculitis barbae) that curl back into the skin after shaving, leading to inflammation, or by a bacterial or fungal infection of the hair follicles (sycosis barbae).
Living with any skin condition can be challenging, and we want you to feel informed and supported. Remember, if you have concerns about your skin, a healthcare professional is the best person to provide guidance.
Sources
- American Academy of Dermatology. (n.d.). Folliculitis. Retrieved from https://www.aad.org/public/diseases/a-z/folliculitis
- Mayo Clinic. (2022, August 31). Folliculitis. Retrieved from https://www.mayoclinic.org/diseases-conditions/folliculitis/symptoms-causes/syc-20361634
- Cleveland Clinic. (2022, October 10). Folliculitis. Retrieved from https://my.clevelandclinic.org/health/diseases/17692-folliculitis