Overview
Lichen Planus (pronounced LIE-ken PLAY-nus) is an inflammatory condition that can affect your skin, hair, nails, and mucous membranes (like the inside of your mouth). It happens when your immune system mistakenly attacks cells of the skin or mucous membranes. While the exact cause isn't always clear, it can be triggered by certain medications, infections (like Hepatitis C), or allergens; sometimes, it just appears without a known reason.
Lichen Planus most commonly affects middle-aged adults, but it can occur at any age. It's important to know that Lichen Planus is not contagious, so you can't catch it from someone else, and you can't give it to anyone. Living with Lichen Planus can be challenging, as the itching and appearance can affect your daily comfort and self-esteem. We understand this can be frustrating, and we're here to help you understand it better.
Symptoms
You might experience a range of symptoms, and they can vary depending on where the Lichen Planus appears. Here are some of the most common signs:
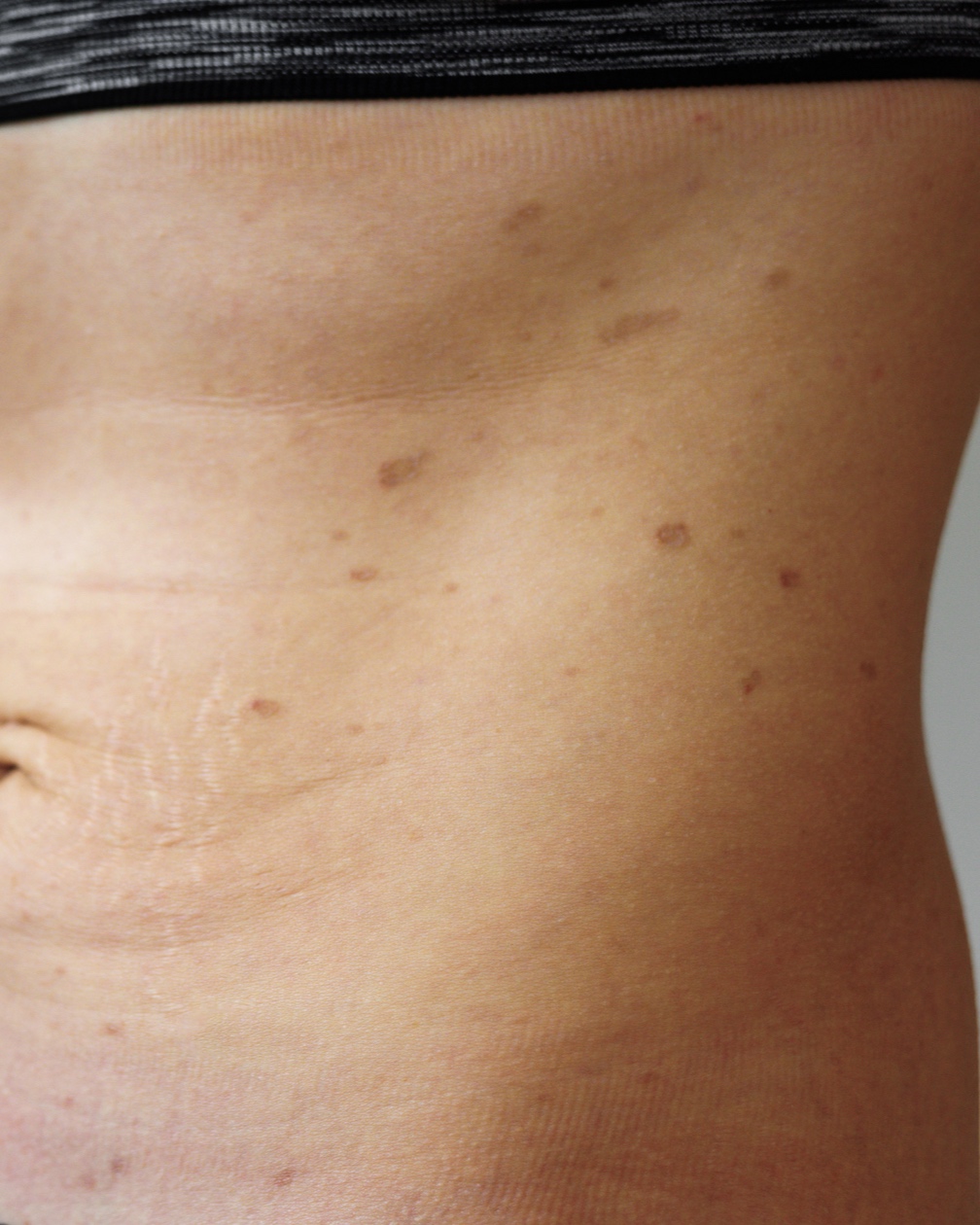
- Purple or reddish-purple bumps (papules) - on your skin, often shiny and flat-topped. These most commonly appear on the wrists, ankles, lower back, and shins.
- Intense itching - at the site of the bumps. This is often the most bothersome symptom for many.
- Lacy white streaks or patches - inside your mouth (oral Lichen Planus), on the tongue, or gums. These might not cause discomfort, but sometimes they can be sore, especially when eating spicy or acidic foods.
- Painful sores or ulcers - in the mouth or on the genitals.
- Thinning, ridging, or loss of nails.
- Hair loss - in patches on the scalp (this is a less common form called Lichen Planopilaris).
- Symptoms can sometimes appear suddenly or develop slowly - over weeks.
- New bumps may appear in lines where the skin has been scratched or injured - (this is called the Koebner phenomenon).
Diagnosis
Figuring out if you have Lichen Planus usually starts with a visit to a healthcare professional, often a dermatologist. They will typically:
- Examine your skin, mouth, nails, and scalp carefully. The appearance of Lichen Planus is often quite distinctive to a trained eye.
- Ask about your medical history - including any medications you're taking or recent illnesses.
- In some cases, a skin biopsy may be needed - to confirm the diagnosis. This involves taking a small sample of the affected skin, which is then examined under a microscope. If oral Lichen Planus is suspected, a biopsy from the mouth lining might be taken.
- Blood tests might be done - to check for conditions sometimes associated with Lichen Planus, like Hepatitis C.
Management & Treatment
Finding the right approach to manage lichen planus can bring you much-needed relief and help your skin, mouth, or nails heal. We know how challenging the itching and discomfort can be, but please know that there are many effective ways to manage this condition. For some people, especially with mild cases on the skin, lichen planus may clear up on its own within a year or two without any treatment.
When treatment is needed, the main goals are to relieve your symptoms, reduce the rash, and help you feel more comfortable.
Home Care and Self-Management Strategies
There are several things you can do at home to help soothe your symptoms:
- For itchy skin: Try applying cool compresses to the affected areas. Taking a lukewarm bath (oatmeal baths can be particularly soothing) and using a gentle, fragrance-free moisturizer can also help. Most importantly, try your best to avoid scratching, as this can make the rash worse.
- For mouth sores: Good oral hygiene is key. Brush gently and avoid spicy, salty, or acidic foods and drinks that might irritate the sores. It's also wise to avoid alcohol and stop smoking.
- Reduce stress: Stress can sometimes trigger or worsen flare-ups. Finding healthy ways to manage stress, like mindfulness, yoga, or gentle exercise, can be a helpful part of your overall care plan.
Over-the-the-Counter (OTC) Options
For mild itching, oral antihistamine pills that you can buy at the pharmacy may provide some relief, especially at night.
Prescription Treatments
If home care isn't enough, a healthcare professional can offer stronger treatments. It's common to need a prescription to get the condition under control.
- Topical Corticosteroids: These are often the first treatment prescribed. They come as creams or ointments that you apply directly to the rash to reduce inflammation and itching. For thicker skin rashes or sores, your doctor might recommend a high-potency steroid.
- Oral Corticosteroids: For severe or widespread lichen planus, your doctor may prescribe steroid pills, like prednisone, for a short time to calm the inflammation quickly.
- Corticosteroid Injections: For stubborn, individual spots, a dermatologist can inject a steroid directly into the lesion to help it heal.
- Immune-Calming Medications: If steroids aren't the right fit or don't work, there are other medications that work by calming the immune system. These can be creams (like tacrolimus or pimecrolimus) or pills (like methotrexate).
- Retinoids: These vitamin A-related drugs, either topical or oral, can also be an effective treatment option.
- Light Therapy (Phototherapy): For widespread rashes on the skin, treatment with a special type of ultraviolet (UV) light can be very effective.
Important Note: If lichen planus affects your scalp (lichen planopilaris), starting treatment early is crucial to prevent permanent hair loss.
When to Expect Improvement
With treatment, you should start to see improvement and feel relief from the itching and discomfort. Skin rashes often respond well and may clear within several months to a year. However, lichen planus in the mouth, on the nails, or on the genitals can be more persistent and may last for several years, sometimes coming and going.
If your symptoms don't improve with the first treatment plan, don't lose hope. It’s very important to follow up with your dermatologist. They can work with you to adjust your treatment, try a different approach, or combine therapies to find what works best for you. Living with lichen planus can be a journey, and your healthcare team is there to support you every step of the way.
Duration & Outlook
The course of Lichen Planus can vary greatly from person to person. For many, skin Lichen Planus typically lasts for several months to a couple of years and then resolves on its own. However, it can sometimes last longer, or it might come and go over time.
Lichen Planus in the mouth (oral Lichen Planus), nails, or scalp can be more persistent and chronic, sometimes lasting for many years. While the condition can be uncomfortable and sometimes distressing, it usually doesn't lead to serious internal health problems. After the skin lesions heal, they might leave behind dark brown or grayish spots on the skin, which can take months or even years to fade.
Warning signs for complications include sores in the mouth that don't heal, significant pain, or difficulty eating. While rare, long-standing erosive oral Lichen Planus has a small risk of developing into oral cancer, so regular check-ups are important.
Prevention
Unfortunately, because the exact cause of Lichen Planus isn't fully understood in many cases, there's no guaranteed way to prevent it from occurring in the first place.
However, if you've been diagnosed with Lichen Planus, you might be able to help manage flare-ups or prevent worsening by:
- Avoiding known triggers if any have been identified for you (like certain medications).
- Reducing stress, as stress can sometimes exacerbate skin conditions.
- For oral Lichen Planus, maintaining good oral hygiene, avoiding tobacco, and limiting alcohol and irritating foods (like very spicy or acidic items) may be helpful.
- Protecting your skin from injury, as new lesions can sometimes appear in areas of trauma.
Causes & Triggers
Lichen Planus is thought to be an autoimmune condition, meaning your body's immune system, which normally fights off infections, mistakenly attacks healthy cells in your skin, hair, nails, or mucous membranes. The precise reason why the immune system does this isn't fully known.
Common triggers or associations can include:
- Certain medications: Pain relievers (like NSAIDs), medications for high blood pressure, heart disease, or arthritis.
- Infections: Hepatitis C infection has a known link to Lichen Planus.
- Allergens: Contact with certain chemicals or dental materials (like mercury fillings, though this is debated and less common).
- Stress: While not a direct cause, stress can sometimes trigger flare-ups or worsen symptoms.
- Genetics: While not strongly hereditary, there might be a slight genetic predisposition in some families.
Who is most likely to develop it?
- Adults between the ages of 30 and 60 are most commonly affected.
- It affects men and women fairly equally, though oral Lichen Planus may be more common in women.
Risk factors include:
- Having other autoimmune disorders.
- Exposure to certain medications or chemicals.
- Having a Hepatitis C infection.
When to see a doctor
It's always best to consult a healthcare professional if you notice any new, unexplained rash or changes to your skin, mouth, hair, or nails. Specifically for Lichen Planus, you should seek medical advice if:
- You develop purple or reddish-purple, itchy bumps - on your skin.
- You notice lacy white patterns, redness, or sores inside your mouth - especially if they are painful or make eating difficult.
- Your nails become thin, ridged, or start to split or fall off.
- You experience patches of hair loss - accompanied by scalp redness or irritation.
- The itching is severe and disrupts your sleep or daily activities.
- You have any sores that don't heal within a few weeks.
A dermatologist is a specialist in skin conditions and is the best type of doctor to see for diagnosing and managing Lichen Planus. They can confirm the diagnosis and discuss appropriate ways to manage your symptoms.
Frequently Asked Questions (FAQs):
- Is Lichen Planus cancerous? Lichen Planus of the skin is not cancerous and does not turn into skin cancer. However, very rarely, long-lasting erosive (ulcerative) Lichen Planus in the mouth or on the genitals can increase the risk of developing a type of skin cancer called squamous cell carcinoma in those areas. Regular check-ups are important if you have this form.
- Will the dark spots left by Lichen Planus ever go away? Yes, the dark spots (post-inflammatory hyperpigmentation) that can remain after skin Lichen Planus heals usually fade over time. However, this can take many months or even a couple of years. Sun protection can help prevent them from darkening further.
- Can stress make Lichen Planus worse? While stress doesn't directly cause Lichen Planus, it can be a trigger for flare-ups or make existing symptoms feel worse for some people. Managing stress through relaxation techniques or other methods may be helpful.
- If I have Lichen Planus in my mouth, do I need to see a dentist? Yes, it's a good idea. While a dermatologist can diagnose and help manage oral Lichen Planus, regular dental check-ups are important for your overall oral health and to monitor the condition. Your dentist and dermatologist can work together.
We hope this information helps you understand Lichen Planus better. Remember, you're not alone in this, and seeking advice from a healthcare professional is a key step in managing any skin concern.
Sources
The content has been successfully updated.