Melanoma is a serious type of skin cancer that begins in cells called melanocytes, which are responsible for producing the pigment that gives skin its color. It is primarily caused by intense, occasional ultraviolet (UV) exposure, especially sunburns, but genetics can also play a role. While melanoma can occur at any age, it's more common in adults with fair skin, a history of sunburns, or a family history of the condition.
Discovering a spot that might be melanoma can be very worrying, and it's a condition we take very seriously because if not caught early, it can spread to other parts of the body, significantly impacting health and quality of life. Early detection is key.
Symptoms
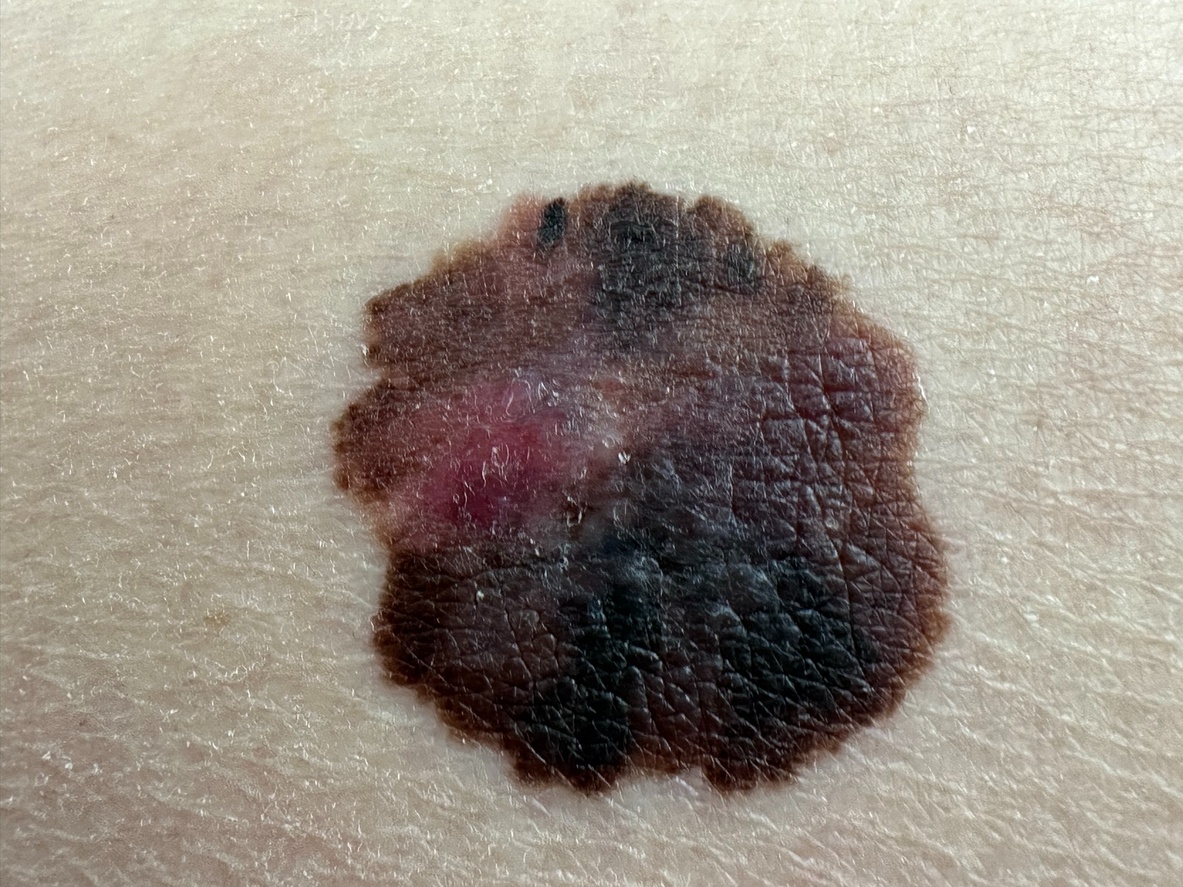
The most common sign of melanoma is a new mole or a change in an existing mole. It's helpful to remember the ABCDEs of melanoma when checking your skin:
- A for Asymmetry: One half of the mole or spot doesn't match the other half.
- B for Border: The edges are irregular, ragged, notched, or blurred.
- C for Color: The color is not the same all over and may include different shades of brown or black, or sometimes with patches of pink, red, white, or blue.
- D for Diameter: The spot is larger than 6 millimeters across (about ¼ inch – the size of a pencil eraser), although melanomas can sometimes be smaller when first detected.
- E for Evolving: The mole is changing in size, shape, color, or elevation. Some melanomas don't fit these rules, so it's important to tell your doctor about any new skin changes or growths that look different from the rest of your moles.
Also look out for these symptoms:
- A sore that doesn't heal.
- Spread of pigment from the border of a spot into surrounding skin.
- Itching, tenderness, or pain in a mole or lesion.
- Bleeding from a mole.
Diagnosis
If you or your doctor suspect a spot might be melanoma, the first step is usually a thorough skin examination. Your doctor will look at the suspicious spot closely, often using a special magnifying tool called a dermatoscope, which helps them see features not visible to the naked eye.
If melanoma is suspected, the only way to make a definitive diagnosis is with a skin biopsy. This involves removing a small sample of the suspicious skin, or the entire lesion if it's small enough, which is then sent to a laboratory to be examined under a microscope by a pathologist. This test will confirm if cancer cells are present and, if so, what type.
Management & Treatment
Hearing you have melanoma can be overwhelming, but it's important to know there are more effective treatments available now than ever before. Your treatment plan will depend on the stage of the melanoma, where it is, and your overall health. Your care team will be your best partner in this journey.
The main goal of treatment is to remove the cancer completely, ideally with surgery. For more advanced cases, treatments work throughout the body to kill cancer cells.
- Surgery: This is the primary treatment for almost all stages of melanoma. The surgeon removes the tumor along with a small margin of surrounding healthy skin. For very thin, early melanomas, the biopsy itself may be enough to remove all the cancer. If the melanoma is deeper, a wider excision is needed. Your doctor may also perform a sentinel lymph node biopsy to check if the cancer has spread.
- Immunotherapy: These are advanced medicines that use your body's own immune system to find and destroy cancer cells. Immunotherapy has dramatically improved the outlook for patients with advanced melanoma and is often used after surgery for later-stage melanomas to help prevent the cancer from returning.
- Targeted Therapy: These drugs are designed to attack specific gene changes in the melanoma cells. If your tumor has a certain mutation (like in the BRAF gene), these pills or capsules can be very effective at shrinking the cancer.
- Radiation Therapy: This treatment uses high-energy rays to kill cancer cells. It may be used after surgery to target the area where lymph nodes were removed or to treat melanoma that has spread to other parts of the body, like the brain.
- Chemotherapy: While it used to be a primary treatment, chemotherapy is less common now for melanoma. It is typically reserved for cases where immunotherapy and targeted therapy are no longer working.
Deciding on a treatment path is a big step, and it's okay to take a moment to understand all your options with your doctor. Most treatments for early melanoma are highly successful. For more advanced melanoma, improvement can take longer, but the newer therapies have given many people long-term control of their disease.
If a treatment isn't working as well as hoped, don't lose heart. The field of melanoma research is incredibly active, and there are often other options to explore, including clinical trials for new and promising therapies. Always maintain open communication with your healthcare team about how you're feeling.
Duration & Outlook
Melanoma is not a condition that will go away on its own; it requires medical evaluation and, if confirmed, treatment. It is considered a chronic concern in the sense that once you've had melanoma, you are at higher risk for developing new melanomas, so lifelong skin checks are very important.
The outlook for melanoma depends heavily on how early it is detected and its thickness. When found and treated in its earliest stages, the outcome is often very good. If melanoma has spread deeper into the skin or to other parts of the body, it becomes more challenging. Warning signs for complications or spread can include the original site becoming lumpy, new unexplained pain, swollen lymph nodes near the melanoma site, or general symptoms like fatigue or unexplained weight loss.
Prevention
While not all melanomas can be prevented, you can significantly reduce your risk. The most important preventive step is to protect your skin from UV radiation.
- Seek shade, especially between 10 a.m. and 4 p.m. when UV rays are strongest.
- Wear protective clothing, including a wide-brimmed hat and UV-blocking sunglasses.
- Use a broad-spectrum sunscreen with an SPF of 30 or higher every day, even on cloudy days, and reapply every two hours, or after swimming or sweating.
- Avoid tanning beds and sunlamps entirely. These are proven to increase melanoma risk.
- Perform regular self-skin exams (monthly) to become familiar with your skin and notice any changes.
- See a dermatologist for regular professional skin exams, especially if you have a higher risk.
Causes & Triggers
The primary cause of most melanomas is exposure to ultraviolet (UV) radiation from the sun or artificial sources like tanning beds. This UV exposure can damage the DNA in skin cells, leading to mutations that can cause cells to grow uncontrollably and become cancerous.
Common triggers and risk factors include:
- History of sunburns: Even one blistering sunburn in childhood or adolescence can more than double a person's chances of developing melanoma later in life.
- Excessive sun exposure: Cumulative sun exposure over time also increases risk.
- Tanning bed use: Increases melanoma risk significantly, especially in younger individuals.
- Many moles: Having 50 or more common moles increases risk.
- Atypical moles (dysplastic nevi): These moles are often larger than common moles, have irregular borders, and varied color.
- Fair skin, light hair, and light-colored eyes: People who sunburn easily are at higher risk.
- Family history of melanoma: Having one or more first-degree relatives (parents, siblings, children) with melanoma increases your risk.
- Personal history of skin cancer: If you've had melanoma or other skin cancers before, you're at higher risk.
- Weakened immune system: Due to medical conditions or medications.
When to see a doctor
It's so important to be proactive about your skin health. You should see a doctor, preferably a dermatologist, if you notice:
- Any new mole or spot that looks different from other spots on your skin.
- A mole or spot that is changing in size, shape, or color (remember the ABCDEs).
- A spot that itches, bleeds, is tender, or painful.
- A sore that doesn't heal.
- Any skin change that worries you, even if it doesn't fit the typical descriptions. It's always better to have it checked.
If you have a high risk of melanoma (e.g., family history, many moles, previous melanoma), regular full-body skin exams by a dermatologist are crucial, often recommended annually or more frequently based on your individual risk. Trust your instincts; if something on your skin feels wrong or looks suspicious, please don't wait to get it checked.
Frequently Asked Questions (FAQs):
- Can melanoma appear suddenly? Yes, melanoma can develop as a new spot on the skin, or it can arise from an existing mole. Some melanomas grow quickly, while others develop more slowly over time.
- Is melanoma always dark or black? While many melanomas are dark brown or black, they can also be tan, pink, red, blue, or even skin-colored (amelanotic melanoma). The key is change or a spot that looks different from your others.
- If I had a mole removed that wasn't melanoma, am I safe? Having a non-cancerous mole removed doesn't increase your risk for melanoma. However, it's still important to monitor all your moles and skin for any new changes and continue sun protection.
- Does melanoma only occur on sun-exposed skin? While melanoma is most common on sun-exposed skin, it can occur anywhere on the body, including areas that get little or no sun, like the soles of the feet, palms of the hands, under fingernails or toenails, and even inside the mouth or eyes. This is why a thorough skin check is so important.
- Is itching a common symptom of melanoma? Itching can be a symptom of melanoma, but not all melanomas itch, and many benign (non-cancerous) skin conditions can also cause itching. If a mole or spot starts to itch, especially if it also has other changes (like in size, shape, or color), it should be evaluated by a doctor.
We understand that thinking about melanoma can be stressful. This information is here to help you understand the condition better. If you have any concerns about a spot on your skin, it's always best to see a healthcare professional or a dermatologist for an accurate diagnosis.
References
- American Cancer Society. (2023). What Is Melanoma Skin Cancer?. Retrieved from https://www.cancer.org/cancer/types/melanoma-skin-cancer/about/what-is-melanoma.html
- The Skin Cancer Foundation. (2023). Melanoma. Retrieved from https://www.skincancer.org/skin-cancer-information/melanoma/
- National Cancer Institute. (2023). Melanoma Treatment (PDQ®)–Patient Version. Retrieved from https://www.cancer.gov/types/skin/patient/melanoma-treatment-pdq
- Mayo Clinic. (2022). Melanoma. Retrieved from https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884