Overview
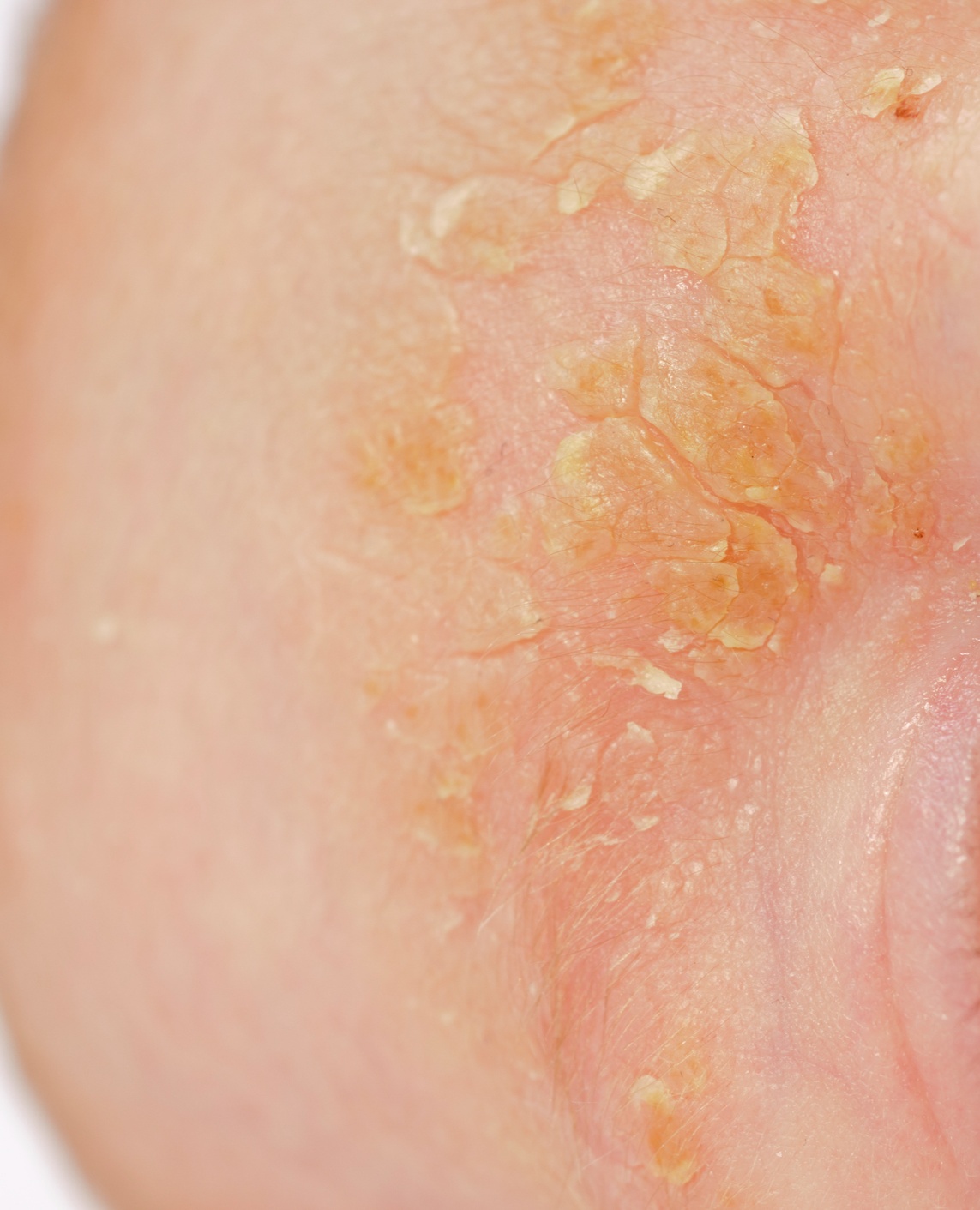
Seborrheic Dermatitis is a very common skin condition that mainly affects your scalp, causing scaly patches, red skin, and stubborn dandruff. It can also affect oily areas of the body, like the face, sides of the nose, eyebrows, ears, eyelids, and chest.
The exact cause isn't fully understood, but it's thought to be linked to a yeast (fungus) called Malassezia that lives on everyone's skin, combined with an inflammatory response, and possibly genetic and environmental factors. It commonly affects infants (often called "cradle cap") and adults, particularly between the ages of 30 and 60. Don't worry, it is not contagious, so you can't catch it from someone else or pass it on. While it can be bothersome and sometimes make you feel self-conscious, it's generally not a serious threat to your overall health.
Symptoms
You might notice a few different things if you have seborrheic dermatitis. Symptoms can vary from person to person and can flare up at times. Here are some common signs:
- Skin flakes (dandruff) on your scalp, hair, eyebrows, beard, or mustache.
- Patches of greasy skin covered with flaky white or yellowish scales or crusts on the scalp, face (especially around the nose, eyebrows, and ears), upper chest, armpits, or groin area.
- Red skin.
- Itching or a burning sensation, which can range from mild to quite intense.
- In infants, it often appears as "cradle cap" – thick, crusty, yellow, or brown scales on the baby's scalp.
- Symptoms may be worse during times of stress or in cold, dry weather.
- The severity can range from mild, barely noticeable flaking to more widespread, inflamed patches.
- Sometimes, in more severe cases on the scalp, there can be some temporary hair shedding.
Diagnosis
Figuring out if you have seborrheic dermatitis is usually straightforward for a healthcare professional.
- How is it diagnosed? A doctor can typically diagnose seborrheic dermatitis by looking closely at the affected skin and asking about your symptoms and medical history. They're looking for the characteristic appearance and locations of the rash.
- Common tests or procedures: Most of the time, no special tests are needed. In rare cases, if the diagnosis isn't clear or if it's not responding to typical approaches, your doctor might suggest a skin scraping to check for fungus or a skin biopsy (taking a small sample of skin) to rule out other conditions that can look similar, like psoriasis or eczema.
Management & Treatment
Finding the right approach to manage seborrheic dermatitis can make a world of difference in your daily comfort and confidence. The main goal is to reduce the visible symptoms, calm inflammation, and control the itching. For many, this is a chronic condition that may come and go, but it can be effectively controlled with consistent care.
In some mild cases, especially in infants, the condition may clear up on its own. However, for most adolescents and adults, a regular skincare routine is needed to manage symptoms and prevent flare-ups.
Over-the-Counter (OTC) & Home Care
For many people, seborrheic dermatitis can be managed well with products you can find at your local pharmacy.
- Medicated Shampoos: For your scalp, the first step is often a medicated dandruff shampoo. Look for active ingredients like pyrithione zinc, selenium sulfide, ketoconazole, salicylic acid, or coal tar. It can be helpful to alternate between two different types of shampoos if one seems to lose its effectiveness.
- Gentle Cleansing: For your face and body, wash the affected areas daily with a gentle cleanser. Some medicated shampoos can also be used carefully on the face and chest; just be sure to rinse thoroughly.
- Soften and Remove Scales: Before shampooing, you can apply mineral oil or olive oil to your scalp for an hour or so to help soften and loosen scales.
- Moisturize: Applying a non-irritating moisturizer after washing can help reduce redness and flaking.
- Lifestyle Adjustments: Managing stress, getting enough sleep, and avoiding known triggers like harsh detergents or cold, dry weather can help prevent flare-ups.
When Prescription Treatments Are Needed
If your skin doesn't improve with self-care and OTC products, it’s time to see a healthcare professional. They may recommend stronger treatments, such as:
- Prescription-Strength Shampoos, Creams, or Gels: These products contain higher concentrations of antifungal agents (like ketoconazole or ciclopirox) to control the yeast on the skin.
- Topical Corticosteroids: Your doctor might prescribe a steroid cream, lotion, or ointment (such as hydrocortisone or desonide) to apply to the affected area. These are very effective at reducing inflammation and redness. Important: Use these only as directed and for short periods, as long-term use can cause side effects like skin thinning.
- Calcineurin Inhibitors: Creams or ointments containing tacrolimus or pimecrolimus are another option. They work by calming the immune system and are a good alternative to steroids, especially on sensitive areas like the face and eyelids.
Improvement can often be seen within a few weeks of starting the right treatment. However, since seborrheic dermatitis can return, you may need an ongoing maintenance plan to keep your skin clear. If a treatment isn't working or if your skin becomes painful, starts to crust, or drains fluid, be sure to follow up with your doctor.
Duration & Outlook
Understanding how long seborrheic dermatitis might last and what to expect can be helpful.
- Typical timeline for condition: Seborrheic dermatitis is often a long-term (chronic) condition. This means it can come and go over many years.
- Is it chronic or acute? For most adults, it's chronic. You might have periods when your skin is clear (remission) and other times when symptoms flare up. In infants (cradle cap), it usually clears up on its own within a few months to a year and doesn't typically return.
- What outcomes to expect: While there isn't a permanent cure for adult seborrheic dermatitis, the symptoms can usually be managed effectively. The goal is to control flare-ups and keep your skin comfortable. It doesn't usually lead to serious long-term health problems.
- Warning signs for complications: It's important to watch for signs of a possible skin infection, such as increased pain, swelling, warmth, significant redness spreading from the affected area, or pus draining from the patches. If you notice these, or if the condition suddenly gets much worse or spreads rapidly, it's a good idea to see your doctor.
Prevention
While you might not be able to completely prevent seborrheic dermatitis if you're prone to it, there are things you can do to help manage it and reduce the frequency or severity of flare-ups.
- How can it be prevented? If you know you're susceptible, focusing on gentle skin and scalp care is key.
- Common triggers and how to avoid them:
- Stress: Try to find healthy ways to manage stress, as it's a common trigger.
- Harsh soaps and detergents: Use mild, gentle cleansers on your skin and scalp. Avoid products with alcohol, as they can be drying and irritating.
- Infrequent washing: Regular, gentle cleansing of affected areas can help reduce oiliness and skin cell buildup.
- Cold, dry weather: These conditions can make symptoms worse.
- Scratching: Try to avoid scratching, as this can irritate the skin further and potentially lead to infection.
Causes & Triggers
Understanding what might be behind seborrheic dermatitis can help you identify things that might make your symptoms flare.
- What causes it? The exact cause isn't fully known, but several factors are believed to play a role:
- Malassezia yeast: This is a type of fungus that normally lives on the skin's oily secretions. In people with seborrheic dermatitis, this yeast may overgrow, or the body may have an overactive inflammatory response to it.
- Inflammatory response: Your body's immune system reaction seems to be involved.
- Genetics: It can sometimes run in families.
- Hormones: Hormonal fluctuations might play a part.
- Common triggers and how to avoid them:
- Stress and fatigue: These are significant triggers for many people.
- Weather extremes: Cold, dry weather often worsens symptoms. However, some people find that hot, humid weather can also be a trigger.
- Oily skin: Having naturally oily skin can make you more prone.
- Infrequent shampooing or skin cleansing: This can allow oils and skin cells to build up.
- Skin care products: Alcohol-based lotions or harsh soaps can irritate the skin.
- Certain medical conditions: People with conditions like Parkinson's disease, epilepsy, HIV/AIDS, or those recovering from stressful medical events like a heart attack are more likely to develop it.
- Some medications: Certain drugs can trigger it as a side effect.
- Who is most likely to develop it?
- Infants, typically within the first few months of life (as cradle cap).
- Adults, most commonly between the ages of 30 and 60.
- It appears to be slightly more common in men than in women.
- Risk factors: Family history of seborrheic dermatitis or other skin conditions like psoriasis, having oily skin, certain neurological and psychiatric conditions, a weakened immune system, and living in a cold, dry climate.
When to see a doctor
While seborrheic dermatitis is common, there are times when it's best to seek professional advice. We care about you getting the right support.
- What signs should you look for?
- If you're very uncomfortable, or the itching is severe and affecting your sleep or daily life.
- If your symptoms are causing you significant embarrassment or anxiety.
- If the condition is widespread or spreading quickly.
- If you suspect a skin infection – look for increased pain, swelling, warmth, pus, or red streaks coming from the affected area.
- If the patches are weeping, oozing, or bleeding.
- If you've tried over-the-counter products for a few weeks and haven't seen any improvement, or if things are getting worse.
- How to know when to see a dermatologist:
- If your primary care doctor is unsure about the diagnosis.
- If the condition is severe and not responding to initial approaches recommended by your primary doctor.
- If you have recurrent flare-ups that you're struggling to manage. A dermatologist specializes in skin conditions and can confirm the diagnosis, rule out other possibilities, and discuss a comprehensive plan to help manage your seborrheic dermatitis. Remember, you don't have to manage this alone.
Frequently Asked Questions (FAQs):
- Is seborrheic dermatitis the same as dandruff? Dandruff is considered a mild, non-inflamed form of seborrheic dermatitis that is limited to the scalp. Seborrheic dermatitis can be more inflamed, red, and can affect other oily areas of the body.
- Can seborrheic dermatitis cause hair loss? Severe or persistent seborrheic dermatitis on the scalp, especially with a lot of inflammation or scratching, can sometimes lead to temporary hair shedding in the affected areas. However, it doesn't usually cause permanent baldness, and hair often regrows once the inflammation is controlled.
- Is seborrheic dermatitis related to diet? While there's no specific diet proven to cure or directly cause seborrheic dermatitis for everyone, some people find that certain foods might trigger or worsen their flare-ups. General good nutrition is always beneficial for skin health. If you suspect a food trigger, it's best to discuss it with your healthcare provider.
- Will seborrheic dermatitis go away on its own? In infants (cradle cap), it very often clears up on its own within a few months to a year. In adults, seborrheic dermatitis tends to be a chronic condition that can persist for years, with periods of improvement (remission) and flare-ups.
- Can stress make seborrheic dermatitis worse? Yes, absolutely. Stress is a very well-known and common trigger for seborrheic dermatitis flare-ups in many people. Learning stress management techniques can be a helpful part of managing the condition.
- Is seborrheic dermatitis an allergy? No, seborrheic dermatitis is not considered an allergic reaction in the typical sense. It's an inflammatory condition, likely involving a reaction to the Malassezia yeast that normally lives on the skin.
References
- American Academy of Dermatology Association. (n.d.). Seborrheic dermatitis: Diagnosis and treatment. Retrieved from https://www.aad.org/public/diseases/a-z/seborrheic-dermatitis-treatment
- Cleveland Clinic. (2022, November 28). Seborrheic Dermatitis. Retrieved from https://my.clevelandclinic.org/health/diseases/14403-seborrheic-dermatitis
- Mayo Clinic. (2022, August 10). Seborrheic dermatitis. Retrieved from https://www.mayoclinic.org/diseases-conditions/seborrheic-dermatitis/symptoms-causes/syc-20352710
- National Eczema Association. (n.d.). Seborrheic Dermatitis. Retrieved from https://nationaleczema.org/eczema/types-of-eczema/seborrheic-dermatitis/