Overview
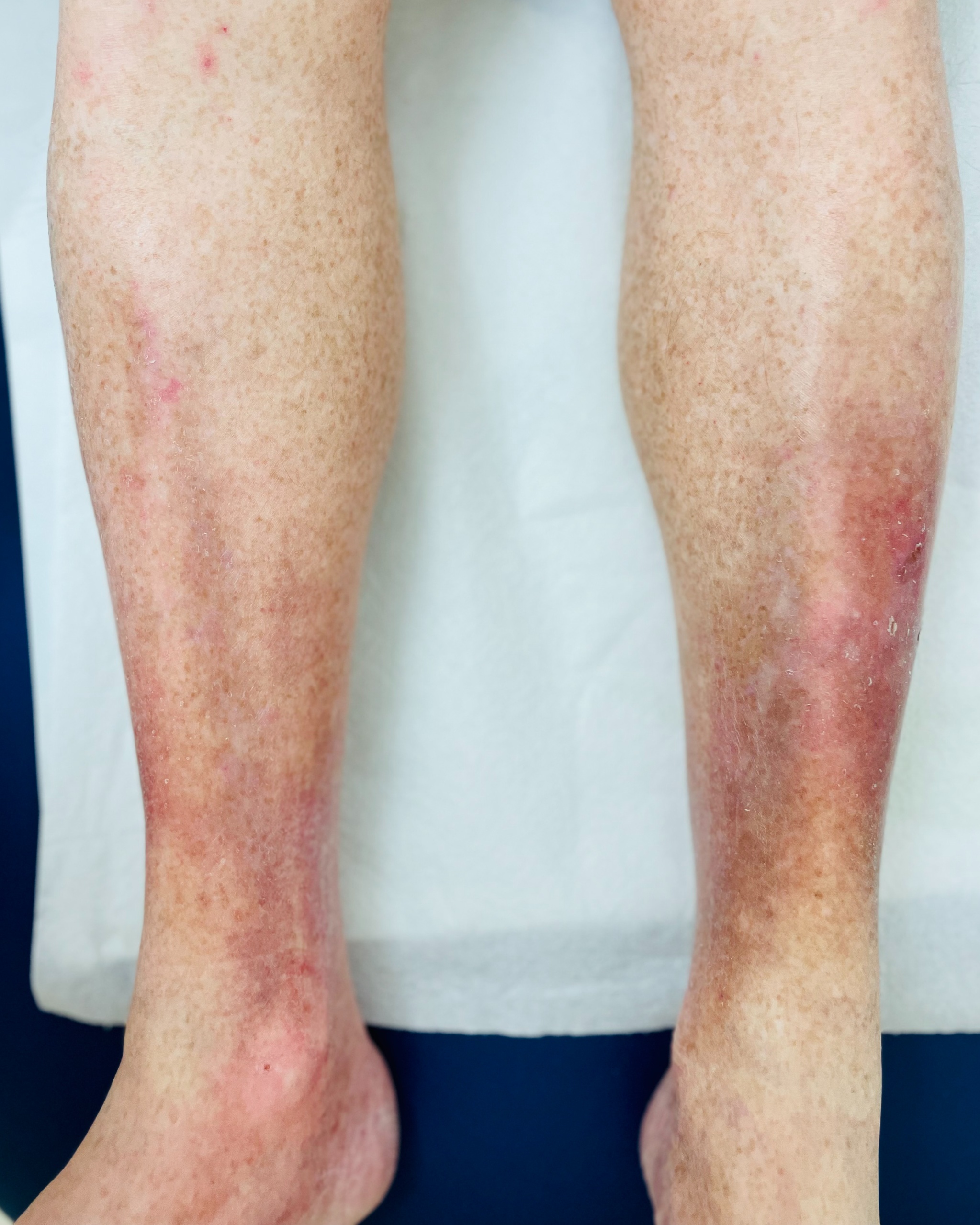
Stasis dermatitis is a type of skin inflammation that occurs in the lower legs. It's caused by poor blood flow (circulation) in the veins, which allows fluid to leak out and collect in the skin and tissues.
It most commonly affects older adults, particularly those over 50, and people with conditions that affect blood flow in the legs, like varicose veins or a history of blood clots. The good news is that stasis dermatitis itself is not contagious, so you can't catch it from someone else, and you can't give it to anyone. Living with stasis dermatitis can be uncomfortable and sometimes frustrating, but understanding it is the first step.
Symptoms
You might notice a few different things if you have stasis dermatitis. Here are some common signs:
- Swelling in the ankles or lower legs, often worse at the end of the day or after standing for a long time.
- Changes in skin color on the lower legs or ankles, which may appear reddish, brownish, or purplish.
- Itching, which can range from mild to very intense.
- Dry, scaly, or cracked skin on the affected areas.
- A feeling of heaviness or aching in the legs.
- Sometimes, small, itchy bumps or even oozing, crusty sores can develop, especially if the skin is scratched.
- The skin may feel thicker or tougher over time (this is called lipodermatosclerosis).
- In more severe cases, open sores called venous ulcers can form, which can be painful and slow to heal.
Diagnosis
A doctor, often a dermatologist, can usually diagnose stasis dermatitis by looking closely at your skin and talking with you about your symptoms and medical history. They'll pay attention to any signs of poor circulation, like swelling or varicose veins.
Sometimes, your doctor might want to do a test called a Doppler ultrasound. This is a painless test that uses sound waves to check the blood flow in your leg veins and see if there are any blockages or problems with the vein valves.
Management & Treatment
We know that managing stasis dermatitis can feel like a constant battle, but please don't lose hope. The goal of treatment is twofold: to heal the skin and to address the underlying circulation problem causing the issue. With the right care, you can significantly reduce your symptoms and prevent the condition from getting worse.
The cornerstone of managing stasis dermatitis is improving blood flow in your legs.
- Leg Elevation: This is one of the simplest and most effective things you can do. Try to elevate your legs above the level of your heart for 15 minutes every 2 hours and while you sleep. This uses gravity to help the fluid drain away from your legs.
- Compression Therapy: Your doctor will likely recommend wearing compression stockings. These special socks apply gentle, steady pressure to your legs, which helps to reduce swelling and improve blood flow. It's important to get the right fit and pressure, so be sure to follow your provider’s guidance.
- Keep Moving: Gentle exercise, like walking, can help improve your circulation. If you have a job that requires a lot of sitting or standing, take frequent breaks to walk around for a few minutes.
Caring for your skin is also crucial to reduce itching and prevent infection:
- Moisturize, Moisturize, Moisturize! The skin in this condition is often very dry. Apply a thick, fragrance-free moisturizer (like petroleum jelly or a cream) throughout the day to keep the skin soft and prevent cracking.
- Topical Steroids: For flare-ups with a lot of redness and itching, your doctor may prescribe a corticosteroid cream or ointment. This helps to calm the inflammation. It’s important to use these only as directed by your provider.
- Medicated Dressings: If open sores or ulcers develop, they need special care. Your provider may recommend specific medicated bandages or dressings to help them heal and prevent infection.
In some cases, if you develop a skin infection (cellulitis), your doctor will prescribe oral antibiotics. It's so important to see your provider if you notice signs of infection like increased redness, warmth, pain, or pus.
Living with a chronic condition takes time and patience. It may take a little while to find the combination of treatments that works best for you. If your symptoms aren't improving, don't get discouraged. Talk with your healthcare provider, as they may refer you to a vein specialist (vascular surgeon) to discuss procedures that can treat the underlying vein problems.
Duration & Outlook
Stasis dermatitis is often a chronic condition, meaning it can last for a long time, especially if the underlying circulation problems aren't managed. While it might not go away completely, the symptoms can usually be managed well with care.
The outlook depends on how well the blood flow issues are addressed and how carefully the skin is cared for. Without proper care, there's a risk of complications like skin infections (cellulitis) or venous ulcers (open sores), which can be slow to heal. Warning signs for complications include increasing pain, redness that spreads, warmth in the affected area, pus or drainage from sores, or a fever.
Prevention
Preventing stasis dermatitis, or stopping it from getting worse, mainly involves improving blood flow in your legs. Here are some things that can help:
- Elevate your legs whenever possible, especially when sitting or lying down. Try to keep them above the level of your heart.
- Wear compression stockings if your doctor recommends them. These special stockings help squeeze your legs gently to improve blood flow.
- Avoid standing or sitting for very long periods without moving. If you have to sit or stand for work, take breaks to walk around.
- Regular exercise, like walking, can help improve circulation.
- If you are overweight, losing weight can reduce pressure on your leg veins.
Causes & Triggers
The main cause of stasis dermatitis is venous insufficiency. This happens when the valves in your leg veins don't work properly, making it hard for blood to flow back up towards your heart. This causes blood to pool in the lower legs, increasing pressure in the veins and allowing fluid to leak into the skin.
Common triggers or factors that can make it worse include:
- Prolonged standing or sitting
- Not elevating the legs
- Injury to the affected area
- Hot weather, which can sometimes increase swelling
Who is most likely to develop it?
- Older adults (over 50)
- People with a history of varicose veins
- Individuals who have had deep vein thrombosis (DVT) or blood clots in their legs
- Those who are overweight or obese
- People with high blood pressure
- Individuals with a history of multiple pregnancies
- Those with heart conditions like congestive heart failure
- People who have had surgery or injury to their legs
Risk factors include increasing age, a family history of vein problems, a sedentary lifestyle, and conditions that affect blood circulation.
When to see a doctor
It's always a good idea to see a doctor if you notice new or worsening skin changes on your legs, especially if you have swelling.
You should definitely make an appointment if you see:
- Skin that is very red, warm, painful, or tender to the touch, as this could be an infection.
- Open sores or ulcers developing on your skin.
- Fluid oozing or crusting on the skin.
- A fever along with skin changes.
- The condition is getting worse despite home care.
- You are unsure what is causing your skin problem.
A dermatologist is a specialist in skin conditions and can provide an accurate diagnosis and discuss management options with you. Don't hesitate to reach out to them; they are there to help!
Frequently Asked Questions (FAQs)
- Is stasis dermatitis painful? It can be. Some people experience aching or heaviness in their legs, and the skin itself can be itchy or tender. If open sores develop, those can be quite painful.
- Will stasis dermatitis spread to other parts of my body? Stasis dermatitis is typically limited to the lower legs and ankles because it's related to circulation issues in that area. It doesn't usually spread to other parts of the body like the arms or trunk.
- Can stasis dermatitis be cured? While the underlying cause (venous insufficiency) is often a long-term condition, the symptoms of stasis dermatitis can usually be managed very well. It's more about ongoing care and management rather than a one-time cure for many people.
- Is it okay to scratch if my skin itches? I know it's so tempting, but try your best not to scratch! Scratching can break the skin, making it vulnerable to infection and potentially leading to sores. If itching is a big problem, please talk to your doctor.
- Are there special soaps or moisturizers I should use? Gentle, fragrance-free cleansers and thick, bland moisturizers are generally best for sensitive skin affected by stasis dermatitis. Your doctor can give you specific recommendations.
References
- National Eczema Association. (n.d.). Stasis Dermatitis: Symptoms, Causes, Treatment. Retrieved from https://nationaleczema.org/types-of-eczema/stasis-dermatitis/
- American Academy of Dermatology Association. (n.d.). Eczema types: Stasis dermatitis diagnosis and treatment. Retrieved from https://www.aad.org/public/diseases/eczema/types/stasis-dermatitis/treatment
- Cleveland Clinic. (2023). Venous Stasis Dermatitis: Causes, Symptoms & Treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/24388-venous-stasis-dermatitis